The COVID-19 Wave Approaches. Connecticut Searches for Ventilators.

Audio By Carbonatix

Hospital workers prepare to test a person - behind the screen - for COVID-19 at the Prescribed Alternative Testing Hub (PATH) in the portico of the Wheeler Building at Stamford Hospital. Appointments for tests are required and spaced five minutes apart. Those seeking testing drive up to the PATH and get out of their car for the test which takes just a couple of minutes. On Friday, the hospital tested 90 people. Courtesy of CTMirror.org
State officials say they are being creative, and ‘scouring the globe’ in advance of the anticipated need for ventilators.
By Mark Pazniokas, Gregory B. Hladky, and Jenna Carlesso, CTMirror.org
Stamford, a city of 130,000 that so often has prospered from its proximity to New York City, is now feeling some of the Big Apple’s pain from the novel coronavirus. COVID-19 patients occupied one-third of the beds in 305-bed Stamford Hospital as of Friday, and 40 already are on ventilators – the most precious commodity of the pandemic.
Before the pandemic, the hospital typically had no more than 10 people hooked up to ventilators on any given day.
While it’s clear the surge of COVID-19 patients is already being felt by hospitals like Stamford, it’s going to get a lot worse. By the time the caseloads hit their peak – now forecast for late April in Fairfield County and a bit later in New Haven and Hartford counties – Connecticut estimates it will need 12,000 hospital beds and 4,000 ventilators.
The state currently has 1,100 ventilators, said Josh Geballe, the state’s chief operating officer.
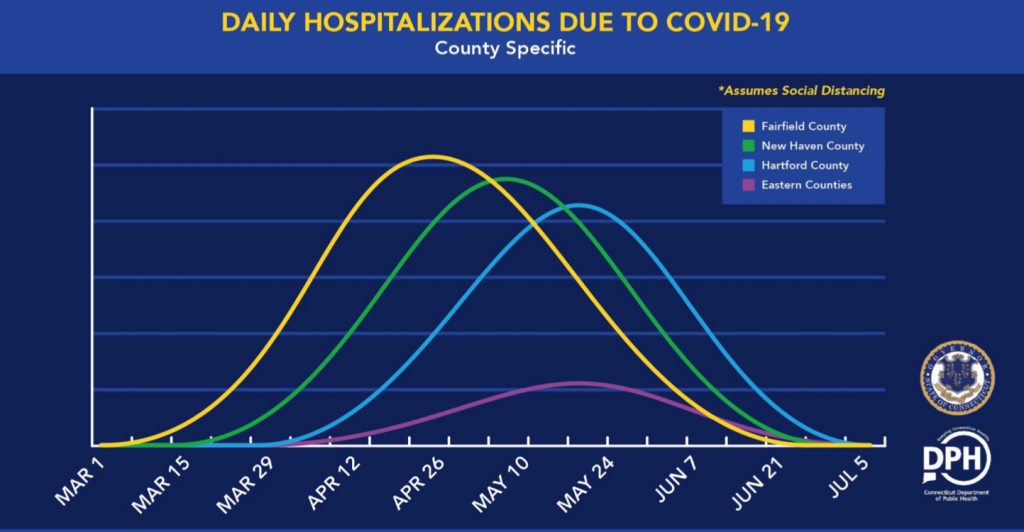
Connecticut expects three major waves of COVID-19 cases, with the first and highest in Fairfield County, (yellow) followed by New Haven (green) and Hartford (blue.) The eastern part of the state could have a lower case load, officials said. Screenshot from Governor Ned Lamont’s press briefing on April 3.
“That is the primary constraint that our health care system is most concerned about,” Geballe said Friday night. “We know we can establish the physical spaces. We have confidence we can fulfill the staffing model. But ventilators are going to be the hardest nut to crack.”
About 45 percent of the 909 coronavirus hospitalizations are in Fairfield County, the slice of Connecticut closest to the pandemic’s center: New York City and Westchester and Nassau counties.
On Friday there were 4,914 laboratory-confirmed cases in Connecticut, with 589 from Stamford, 435 from Norwalk, 402 from Danbury, and 189 from Greenwich. In Saturday’s report, the total number of cases had increased to 5,276, and of those there were 604 in Stamford, 464 in Norwalk, 418 in Danbury, and 191 in Greenwich.
West Hartford’s total number of laboratory-confirmed cases increased to 36 on Friday, and was changed in Saturday’s report.
On March 6, exactly four weeks ago, Gov. Ned Lamont went to Danbury Hospital for a press conference about the first positive test in Connecticut: A New Yorker employed as a health care provider who works at Danbury and Norwalk hospitals. Two days later, the first Connecticut resident was diagnosed.
Geballe said hospital capacity steadily has increased as Connecticut planned for the coming peak by converting spaces to patient rooms and singles into doubles, lowering the non-COVID-19 patient census, and acting creatively to make the most of equipment and supplies.
“The innovation engine in our hospital system is working overtime right now,” Geballe said.
Hospitals are altering some ventilators so they can be used by more than one patient, and gowns and masks go further in wards where there are only COVID-19 patients.
Ben Wade, Stamford Hospital’s senior vice president of strategy, said gowns are in the shortest supply, but so far the hospital is meeting the staff’s needs for other types of personal protection equipment, or PPE.
“We are carefully investigating the efficiency of reusing certain types of PPE and encouraging reuse when it’s deemed safe and clinically appropriate by the CDC and our infectious disease physicians,” Wade said.
Grouping the COVID-19-positive patients also has helped. Medical staff who care for only those patients don’t need to switch out their gear as often.
“If you have, for example, six COVID-19 patients doubled up in three rooms, you don’t need to change gowns,” Wade said. “As you move from room to room, you just need to make sure that you are changing gloves. So there are a lot of things we’re doing – all according to CDC guidelines – that are lowering the demand.”
Stamford Hospital moved into a new $450 million facility in 2016, and now state officials are exploring the feasibility of reopening the old and vacant facility known as the Wheeler Building. They plan to inspect the old hospital building over the weekend.
The hospital is working to bring more critical care nurses, respiratory therapists and other personnel on board.
“We’ve done some creative things. We’ve taken people who traditionally work in an outpatient setting – so, let’s say in our medical group – and brought them in to do jobs that they’re trained to do and appropriately credentialed to do inside the hospital,” Wade said. “We’ve had members of our medical staff, a couple dozen, come in and are working in the hospital now.”
It has been difficult to get a thorough account of the preparedness level of the state’s hospitals and nursing homes. Some staff members say they have been discouraged from talking to reporters, and many hospital officials either decline or do not respond to requests of interviews. Officials at the Connecticut Hospital Association, which is helping to lead the state’s coordinated response to the pandemic, did not grant a request for an interview Friday.
But a number of Connecticut nurses interviewed in recent days on the condition they not be identified said that while supplies of critical equipment are adequate at the moment, the prospect of what is coming, and even the early conservation efforts, are making the hospitals a tense place to work.
“It is very stressful,” said one nurse who works at a Hartford-area hospital. “We don’t have the resources.”
“In an effort to conserve supplies, you’re going to end up getting your whole staff sick, and the staff is going to get all of their patients sick,” warned a nurse at Backus Hospital in Norwich, part of the Hartford Health Care system.
Their not-for-attribution comments are largely consistent with on-the-record statements by leaders of organizations that represent nurses and other health care workers. Anne Hulick, a spokeswoman for the Connecticut Nurses Association, said fear and stress are endemic.
“The biggest thing I’ve heard is the fear, not only of contracting the disease, but also of transmitting it to their families or loved ones when they go home. We’ve heard nurses say they’ve never been scared in their careers, and they are now. So I think the emotional toll, not only the physical toll, of working in healthcare now is so stressful,” Hulick said. “This just adds another layer of physical and emotional stress. What we’re urging the governor to think about is long-term measures that can support nurses and frankly, all health care professionals, on the front lines that are dealing with this incredible added stress.”
Tracy Wodatch, president of Connecticut Association for Healthcare At Home, a trade group representing providers of hospice, home and community health care, said her members are bracing for the surge in cases.
“Currently, most of our providers do have some PPE,” Wodatch said. “The big fear is the surge.”
Hospital and state officials are continuing to search for critical N95 respirator masks, surgical masks, protective gowns, gloves and other protective equipment.
As of Thursday, the state had purchased of 2.25 million N95 respirator masks, 2 million surgical masks and 1.45 million disposable face shields. Altogether, the state has ordered $21 million worth of critical medical equipment to deal with the pandemic. Some the orders have arrived, though no specifics were available Friday night.
Geballe said the state is a backstop, not the main supplier of PPEs and other medical equipment.
“The hospitals have their own supply chains. They are acquiring their own supplies, as are many others. The state’s role is to supplement and fill in gaps,” Geballe said.
Connecticut uses a cloud-based tool called Web EOC that allows municipalities, hospitals, emergency responders and others to centrally share information about their needs.
“When they have a need, they feed it up into Web EOC,” Geballe said.
A small committee that includes public health and medical professionals from the Department of Public Health, plus emergency response team members, confer daily to assess the greatest needs not being met by the standard supply chains.
“They prioritize where are the greatest needs, then make the distribution decisions,” Geballe said. Deliveries are made by the National Guard.
UConn Health is making a public appeal for donations of PPE in a public-service announcement on television, adding to the general impression that the need still exceeds supply.
“Most of our providers don’t have enough N95 masks,” Wodatch said, adding the need varies from provider to provider. “It’s sporadic … Some have an adequate supply for now, others have only a few.”
Wodatch said she is aware that some home health care staffers have come down with the coronavirus. “It’s hard to stay away from it as much as you try,” she said.
She doesn’t know how many home health care workers and nurses have COVID-19 and doesn’t believe there is any system in place yet to track that number statewide or to find out what patients served by home health care have contracted the disease.
“Daily, every staff member is screened,” Wodatch said, having their temperature and possible symptoms checked and answering questions about possible contacts with COVID-19 patients.
Wodatch said her organization is collaborating closely with all the other hospital, nursing and medical associations in Connecticut, and confers regularly with state health officials.
Home health care providers are scheduled to receive more PPE through the state. “We’re on the list,” she said, adding that home health care workers are considered Level 1 employees, along with hospital and nursing home staffs and first responders.
Wodatch said state officials are expecting another big shipment of PPE into Connecticut by the end of the week and have promised that some portion of that material will be distributed to home health care providers.
“When you look at the numbers, at what’s going on in New York … all providers are worried and trying to prepare as best they can,” Wodatch said.
“But we don’t know what’s going to happen,” she said.
Reprinted with permission of The Connecticut Mirror. The authors can be reached at [email protected] and [email protected]
Information specific to West Hartford was added by Ronni Newton, We-Ha.com.
Like what you see here? Click here to subscribe to We-Ha’s newsletter so you’ll always be in the know about what’s happening in West Hartford!